abnormal pap smears during pregnancy
 Abnormal Pap Smear Tests: What to Do Next | OB-GYN Women's Centre
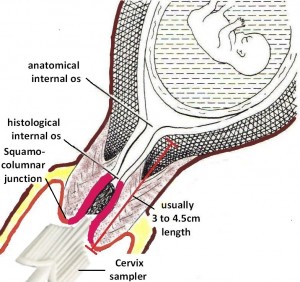
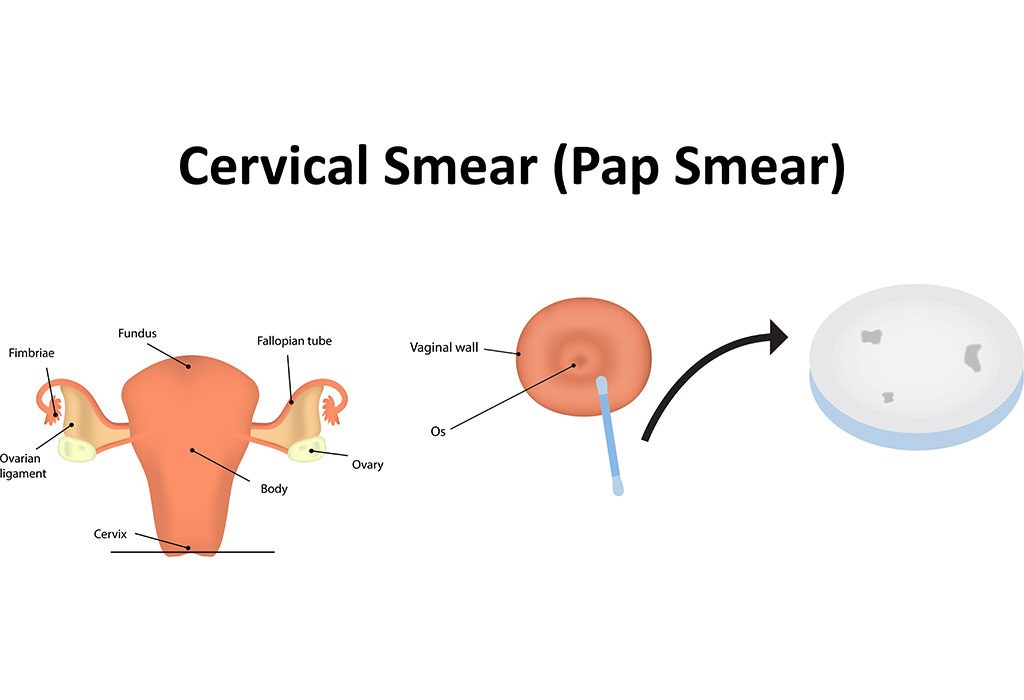
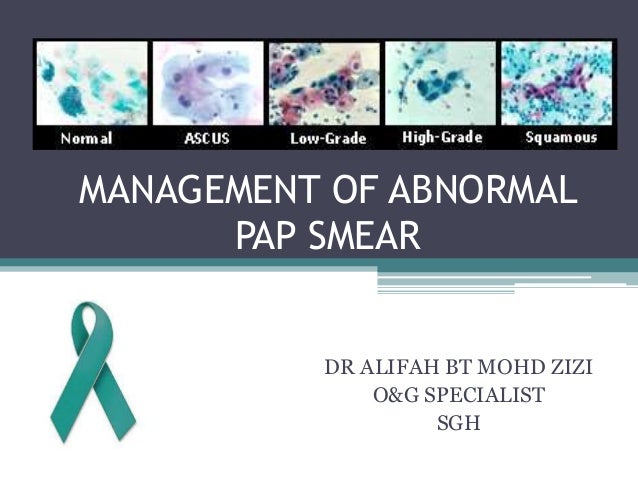
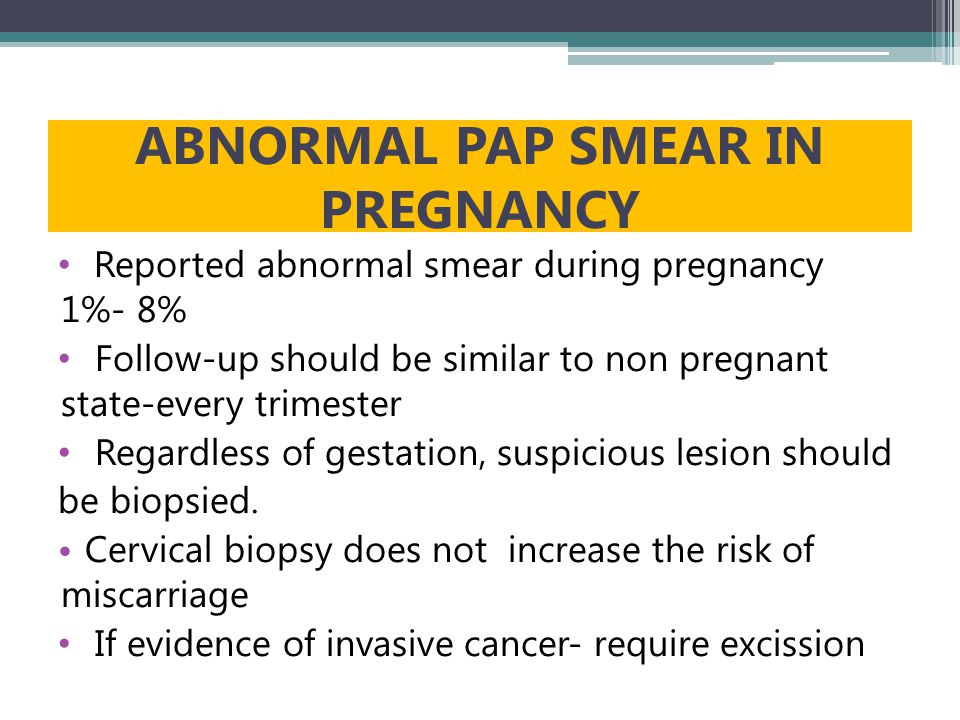
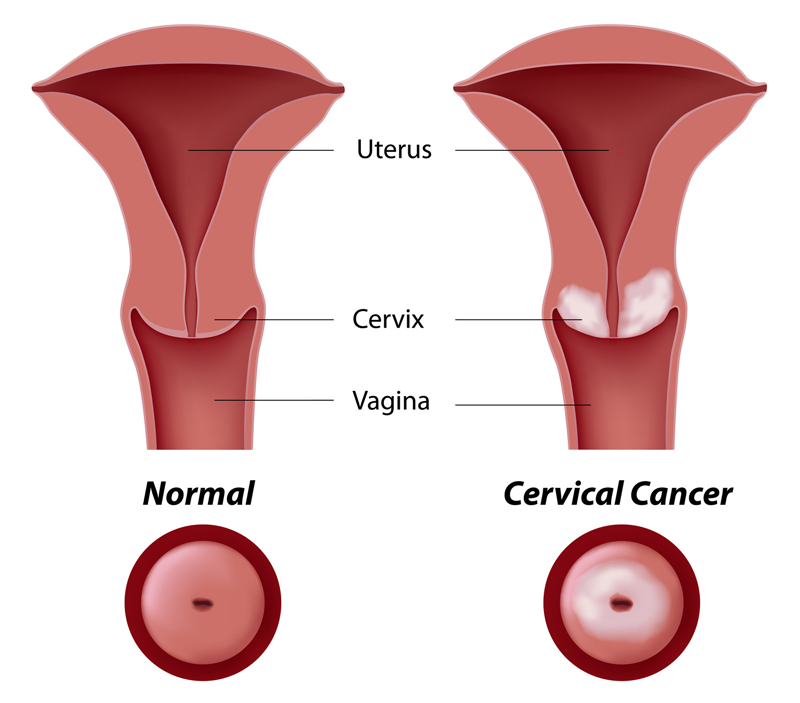
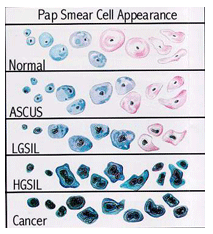
Abnormal Pap Smear Tests: What to Do Next | OB-GYN Women's CentrePregnancy and abnormal cervical cells Before you become pregnant you should check that you are up to date with your cervical exam. If you are already pregnant, you can wait and have the test 3 months after you have had your baby. For women who are pregnant and have an abnormal screening test will depend on the result of your test as to what happens next. Most women may have a normal pregnancy after treatment for abnormal cells, but there are rarely problems. You may need treatment to keep future pregnancies safe. The NHS Cervical Screening Program says routine cervical screening tests can usually be delayed in pregnant women until after having had their baby. Pregnancy can make the test result more difficult to interpret and could be inaccurate. Planning to become pregnant If you are planning to become pregnant, it is a good idea to check with your GP that you are up to date with your cervical exam. Then you can have the test and if you need treatment you can have it before you become pregnant. She's already pregnant. If you are already pregnant, and due to a cervical screening test, you can usually wait to have the test up to 3 months after your baby is born. When you are invited for your test, you should let your GP or clinic know you are pregnant. Then you can delay the test. If you have previously had an abnormal result of a cervical screening test, or have not had a screening test in the last 3 to 5 years, you may need to have a screening test while you are pregnant. Your GP or midwife may ask you to have the test on your first prenatal appointment. This test is safe when you are pregnant. If the results become abnormal, or if a test you had just before you become pregnant shows abnormal results, you don't need to worry. This does not mean that you have cancer, but that there are some abnormal cells that can be treated easily a few months after birth. You may need to have a colposcopy (a close examination of your cervix and vagina) while you are pregnant. This is safe to have during pregnancy, and your doctor can see how much cells have changed in your cervix. Treatment for abnormal cells during pregnancyRemember that if your doctor tells you that you have abnormal cervical cells (or CIN 1, 2 or 3), you do not have cervical cancer. Some of the abnormal cells could become cancer if it is not treated. Before giving birth If you only have mild changes in your cervix cells (INC 1), you will not need to have any treatment up to about 3 months after your baby is born. After that, you may have another colposcopy to check the cervical cells again. In many women with mild changes, they return to normal without any treatment. If the cells are more abnormal (CIN 2 or 3), your doctor may ask you to have another colposcopy when you are pregnant for about 6 months to monitor them. Abnormal cells cannot change much with the time of your pregnancy. If you are pregnant and your colposcopy shows that cell changes have begun to become cancer, your doctor will need to take a tissue sample. This is probably by a procedure called LLETZ (large loop excision of the transformation zone). But your specialist won't do this unless it's absolutely necessary. After giving birth If your cervix cells have not returned to normal after you have given birth, then you may have treatment to remove them. You may discuss your treatment options and any concerns you have with your GP or midwife, or your doctor or nurse specializing in the colposcopy clinic. It's important to make sure you go to all your follow-up appointments after you have had your baby. Pregnancy after a cone biopsy A cone biopsy extracts a wedge of cone tissue in the form of a dye from your cervix. It can cause particular problems with future pregnancies. But they're not common. Ask your doctor how much tissue was removed. If less than 10 mm (1cm) were removed, then it should not cause problems. If more than 10 mm were removed, then in pregnancy they can control your cervix. Reducing the cervixAfter a cone biopsy, there is a very small possibility that the cervix can be narrowed. This is called cervical stenosis. The cervix could be so closed that the sperm cannot enter. If this happened, you wouldn't be able to get pregnant naturally. If you have periods after a cone biopsy you don't have complete cervical stenosis. If the lining of the uterus can come out when it spills like a period, then the sperm can enter. Some women may need surgery to stretch (size) the cervical opening. Future Pregnancies Some NCD treatments or early stage cancer (Page 1A) may cause a small risk of complications in future pregnancies. Women who have had a cone biopsy have: You may have a higher risk of early birth because the cone biopsy has weakened your cervix. The cervix is really a muscle that keeps the entry to the uterus closed unless you are at work. In some women who have had a cone biopsy, there is a risk that the cervix will start opening too soon due to the weight of the growing baby. Serious problems can generally be prevented. If your doctor thinks that your cervix may start opening too soon, he may have a kind of operating point placed around him to keep it closed. Your doctor may call this a portfolio chain suture. The point is cut before going to work, usually a week 37 of your pregnancy. The cervix can be opened normally for the baby to come out. Pregnancy after another treatment It is very unlikely that any other treatment for abnormal cells, such as laser therapy, cold coagulation or cryotherapy will affect your ability to become pregnant in the future. The most likely way these treatments can affect your ability to become pregnant, is if you receive an infection after treatment that spreads in your fallopian tubes. The infection in the fallopian tubes can make them block. If both tubes are blocked, then their eggs cannot travel through the tubes in their belly. This would mean you couldn't get pregnant naturally. Such severe infection is unlikely after treatment for abnormal cells. See your GP immediately if you have symptoms of infection. These may include:LETZAs with cone biopsy, pregnancy studies after LLETZ show that there is a small increase in birth risk before 37 weeks and having a low-weight baby at birth. This risk may depend on the amount of cervical tissue that has been eliminated. There is also a slight increase in the risk that your waters will break early (premature membranes) if you have had LLETZ treatment. If you are pregnant, you should tell your midwife or doctor if you have had treatment for abnormal cervical cells. What to remember You may feel worried about these risks, but remember: 3rd edition Public Health England, 2016 (Updated Feb 2020). Adverse obstetric results after local treatment for cervical pre-invasive disease and early invasive according to cone depth: systematic review and meta analysis M Kyrgiou et al. BMJ, 2016. Volume 354, Number 3633 The risk of premature birth after treatment of premature changes in the cervix: systematic review and meta-analysis F Bruinsma and M Quinn BJOG: International Journal of Obstetrics and Gynaecology, 2011. Volume 118, Number 9Premature birth after treatment of cervical intraepithelial neoplasm among women attending colposcopy in England: retrospective-prospective cohort study A castanon and others BMJ, 2012. Volume 345, Number 5174 Related Content Related Links We know that it is a worrying moment for people with cancer, we have information to help. About cancer generously supported by 2010. Find a Clinical TrialSearch our clinical trial database for all cancer trials and studies that are contracted in the UK Chat forumCancer Talk to Other People Affected by CancerNurse helpline 0808 800 4040 Questions about Cancer? Call the free phone from 9 to 5 Monday to Friday or Follow us 0808 800 4040

Pap and HPV tests | womenshealth.gov
Risk of Miscarriage from a Pap Smear? | Obstetric Excellence
Pap Smear Test during Pregnancy: Need, Safety & Risks Associated

Pap Smear Test during Pregnancy: Need, Safety & Risks Associated

Abnormal Pap Smears - Cherokee Women's Health

Pap smear: What is it, what happens, and results

Figure 1 from Cervical cancer screening in pregnancy. | Semantic Scholar
Pap Smear Test | Cervical Cancer Screening | IVF Infertility Center India
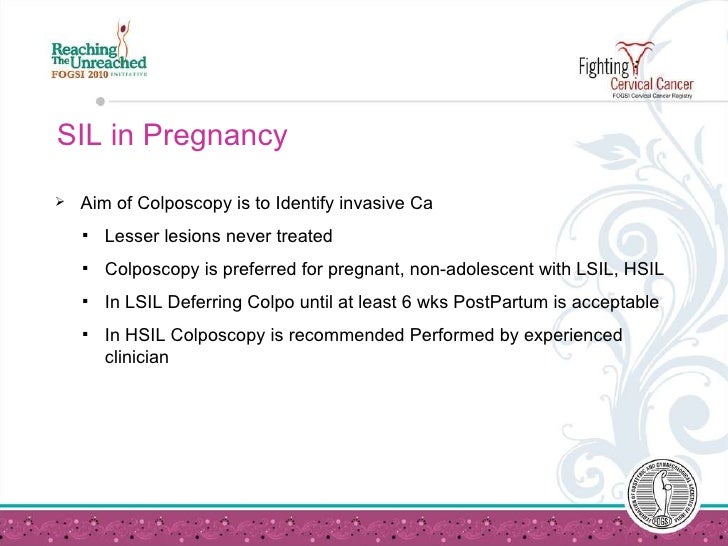
Cervical Cancer Screening in Pregnancy
/3132772_color1-5bc49ccdc9e77c0052898697.png)
Overview of the Pap Smear Procedure
Management of abnormal cervical smear

Figure 4 from Atypical Papanicolaou smear in pregnancy. | Semantic Scholar
Information: Women's Health, Fertility, Pregnancy & Menopause | Yap Specialist

An Abnormal Pap Test Result During Pregnancy?
MANAGEMENT OF ABNORMAL PAP SMEAR - ppt video online download
Pap Test (Papanicolaou Smear) - Harvard Health
.jpg)
Good Reasons to Stop Delaying Your Pap Smear
Understanding HPV and Pap Test Results - National Cancer Institute
Abnormal Pap Smear: Causes and Next Steps | Health.com
Abnormal Pap Smear - International Women's Clinic
Cervical screening during pregnancy | Pregnancy Birth and Baby

Abnormal Pap | HPV in Queens & Long Island, NY | The Woman's Health Pavilion

Abnormal Pap During Pregnancy - ModernMom
/doctor-holding-cervical-smear-equipment-758310077-5c128a53c9e77c000141172a.jpg)
Can a Pap Smear Cause a Miscarriage?
Abnormal Pap Smears – VBGYN.com

New cervical cancer guidelines start making Pap smears obsolete

PDF) Prevalence of abnormal Pap smear during pregnancy in a teaching hospital in South India

Pap test - Wikipedia

No Need To Panic For The Results Of An Abnormal Pap Smear Test? - 2Article
Abnormal Pap Smear Results? What That Really Means & What Comes Next | SELF

Pap Smear Malaysia, Pap Smear - DTAP Clinic for Women in Malaysia

Pap smears may offer early peek at birth defect risk

Smear test: Answers to all your questions about smear tests
Abnormal Pap Test
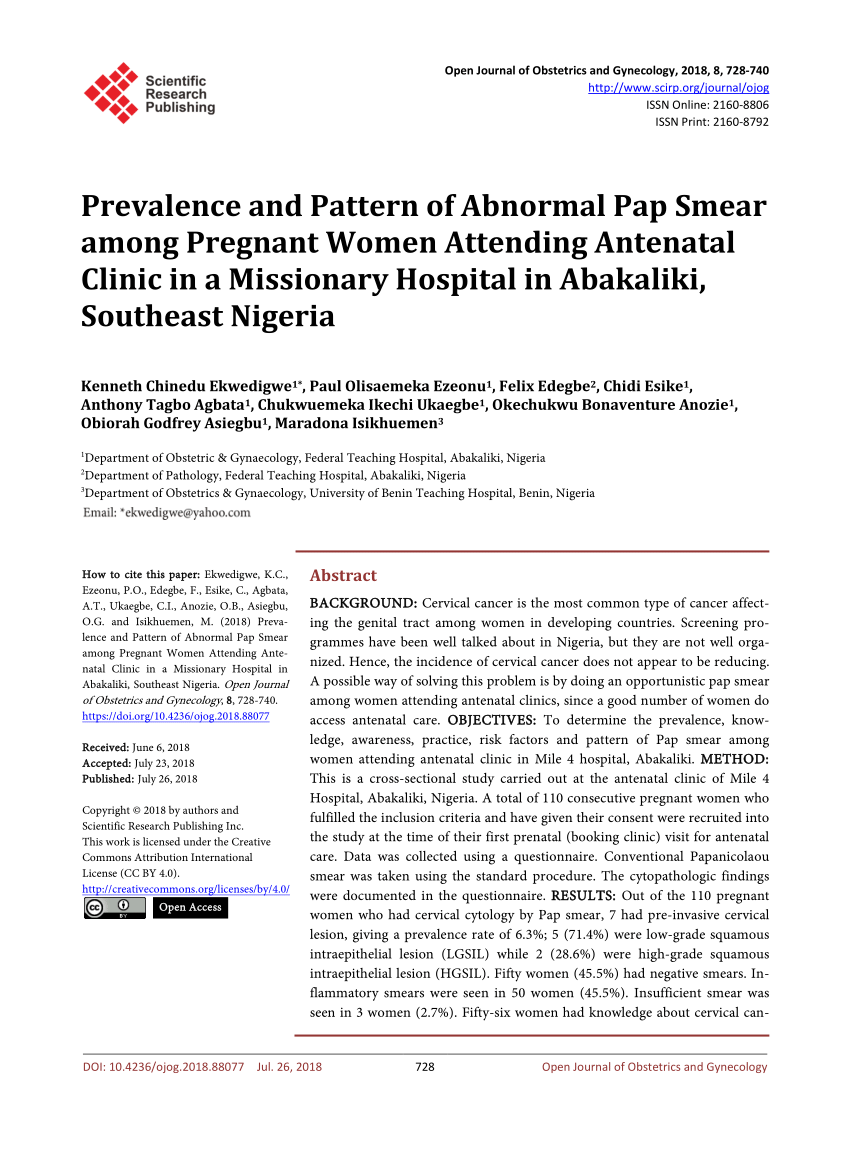
PDF) Prevalence and Pattern of Abnormal Pap Smear among Pregnant Women Attending Antenatal Clinic in a Missionary Hospital in Abakaliki, Southeast Nigeria

What Is a Pap Test & What Can It Tell Me About My Pregnancy?

colposcopy - August 2019 Babies | Forums | What to Expect

My Pap Smear Was Abnormal. Should I Be Worried? - Sharecare

Abnormal Pap Smear Treatment | Best Gynecologists in Brooklyn
Pap Smear Test - What is a Pap Smear, What it tests for, and more
Posting Komentar untuk "abnormal pap smears during pregnancy"